Introduction. The efficacy of CAR T-cell therapy in relapsed/refractory (r/r) LBCL has been associated with peak CAR T-cell expansion post-infusion. One of the critical factors that drives CAR T-cell expansion is the availability of homeostatic cytokines, such as IL-15, at the time of infusion. Consistent with this hypothesis, serum IL-15 levels have been associated with CAR T-cell therapy expansion and efficacy, higher levels favoring improved outcomes. Since induction of lymphodepleting conditioning (LDC) therapy results in decreased consumption of homeostatic cytokines and thereby increases their serum levels, we aimed to determine whether the magnitude of change in absolute lymphocyte count (ALC) pre- and post-conditioning, referred to as delta lymphocyte index (DLIx), impacts outcomes after CAR T-cell therapy in r/r LBCL.
Methods. This is a retrospective study of all patients with r/r LBCL treated with standard of care (SOC) axicabtagene ciloleucel (axi-cel) at MD Anderson Cancer Center between 01/2018 and 04/2020 (data cut-off 06/30/2020). DLIx was defined as the difference in ALC between day of initiation of LDC and day of axi-cel infusion. All patients received LDC therapy with cyclophosphamide and fludarabine. CRS and ICANS were prospectively graded according to CARTOX criteria from 01/2018 to 04/2019, and ASTCT criteria from 05/2019 onward. Response to treatment and progression were defined according to 2014 Lugano criteria.
Results. All 171 LBCL patients treated with SOC axi-cel were included in the analysis. At time of initiation of LDC, median age was 59 years (range, 18-85 years), 120 (70%) were male, 151 (88%) had an ECOG performance status of 0-1; 96 (56%) had an IPI > 3, median number of prior systemic therapies was 4 (range, 2-15), 45 (26%) had received an autologous SCT, 3 (2%) an allogeneic SCT; 86 (50%) patients received bridging therapy, including chemotherapy in 52 (30%), radiotherapy in 21 (12%), and biological therapy or corticosteroids in 13 (8%).
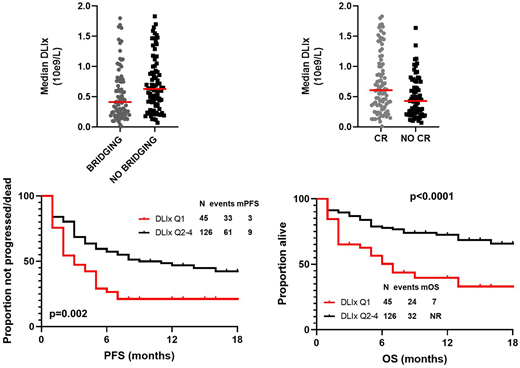
Median ALC at time of LDC was 0.6 X 109/L (range, 0-2.8 X 109/L) and < lower limit of normal (LLN) in 131 (77%) patient; at time of axi-cel infusion it was 0.03 X109/L (range, 0-1.9 X109/L), and median DLIx was 0.5 X 109/L (range, 0.01-2.75 X 109/L). Ten (6%) patients experienced a delay between LDC and axi-cel infusion, with a median time of 13 days (range, 7-19 days), but no association between delay and DLIx was observed (p=0.79). On univariate analysis, the baseline characteristics associated with low DLIx were ALC < LLN (p<0.001), platelet count < LLN (p=0.003) and use of bridging therapy (p=0.02). On MVA, only the association between low DLIx and use of bridging therapy was maintained (Odds Ratio 0.4, 95% 0.2-0.8, p=0.007)(Figure), whereas the association with ALC < LLN was not maintained.
Overall, 13 (8%) patients had grade (Gr) 3-4 CRS, and 61 (36%) had Gr 3-4 ICANS. There was no association between DLIx and incidence of Gr 3-4 CRS (p=0.28) or Gr 3-4 ICANS (0.43).
Of 164 patients evaluable for response, complete responses (CR) was achieved in 89 (54%) patients, and DLIx was significantly higher in patients who achieved CR vs. non-CR (p=0.04)(Figure).
After a median follow-up of 9 months (95% CI, 7-11 months), 94 patients progressed and/or died, and median progression-free survival (PFS) was 6 months (95% CI, 4-8 months). Median PFS was significantly shorter in patients with low DLIx (Q1 vs. Q2-4): 3 months vs 9 months (p=0.002). The association was maintained also after adjusting for bridging therapy use (Hazard Ratio (HR) 0.6, 95% CI 0.4-0.9; p=0.02)(Figure). At data cut-off, 56 (33%) patients died and median OS was not reached. Median OS was significantly shorter among patients with low DLIx (Q1 vs Q2-4) (7 months vs not reached, p<0.001). The association was maintained after adjusting for bridging therapy use (HR 0.4, 95% CI 0.2-0.7; p=0.001) (Figure).
Discussion. DLIx has prognostic value in patients with r/r LBCL treated with axi-cel, with low DLIx independently associating with worse outcome. Additional studies are planned and will be presented to determine whether the pharmacokinetics of cyclophosphamide and fludarabine or other host factors impact DLIx, and whether levels of homeostatic cytokines correlate with DLIx. Such studies could lead to optimization of conditioning therapy and development of future combination strategies, aimed at improving CAR T-cell efficacy in these patients.
Lee:Takeda: Research Funding; Celgene: Research Funding; Guidepoint Blogal: Consultancy; Oncternal Therapeutics: Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Aptitude Health: Speakers Bureau; Seattle Genetics: Research Funding. Iyer:Legend Biotech: Consultancy; Daiichi Sankyo: Consultancy; Seattle Genetics, Inc.: Research Funding; Merck: Research Funding; Afffimed: Research Funding; Trillium: Research Funding; Curio Biosciences: Honoraria; CRISPR: Research Funding; Spectrum: Research Funding; Rhizen: Research Funding; Target Oncology: Honoraria. Nastoupil:Pfizer: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Merck: Research Funding; Karus Therapeutics: Research Funding; TG Therapeutics: Honoraria, Research Funding; LAM Therapeutics: Research Funding; Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Gilead/KITE: Honoraria; Gamida Cell: Honoraria; Genentech, Inc.: Honoraria, Research Funding; Bayer: Honoraria. Parmar:Cellenkos Inc.: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties, Research Funding. Wang:Juno: Consultancy, Research Funding; Kite Pharma: Consultancy, Other: Travel, accommodation, expenses, Research Funding; Pulse Biosciences: Consultancy; OMI: Honoraria, Other: Travel, accommodation, expenses; AstraZeneca: Consultancy, Honoraria, Other: Travel, accommodation, expenses, Research Funding; Dava Oncology: Honoraria; InnoCare: Consultancy; Oncternal: Consultancy, Research Funding; Nobel Insights: Consultancy; Guidepoint Global: Consultancy; Targeted Oncology: Honoraria; Molecular Templates: Research Funding; OncLive: Honoraria; VelosBio: Research Funding; Celgene: Consultancy, Other: Travel, accommodation, expenses, Research Funding; Pharmacyclics: Consultancy, Honoraria, Other: Travel, accommodation, expenses, Research Funding; Janssen: Consultancy, Honoraria, Other: Travel, accommodation, expenses, Research Funding; BioInvent: Research Funding; Beijing Medical Award Foundation: Honoraria; Lu Daopei Medical Group: Honoraria; MoreHealth: Consultancy; Acerta Pharma: Research Funding; Verastem: Research Funding; Loxo Oncology: Consultancy, Research Funding. Shpall:Takeda: Other: Licensing Agreement; Magenta: Membership on an entity's Board of Directors or advisory committees; Adaptimmune: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Zelluna: Membership on an entity's Board of Directors or advisory committees. Kebriaei:Pfizer: Other: Served on advisory board; Ziopharm: Other: Research Support; Amgen: Other: Research Support; Jazz: Consultancy; Novartis: Other: Served on advisory board; Kite: Other: Served on advisory board. Westin:Genentech: Consultancy; Novartis: Consultancy; Janssen: Consultancy; Curis: Consultancy; 47 Inc: Consultancy; Kite: Consultancy; Juno: Consultancy; MorphoSys: Consultancy; Unum: Consultancy. Neelapu:N/A: Other; Takeda Pharmaceuticals: Patents & Royalties; Karus Therapeutics: Research Funding; Pfizer: Other: personal fees; Novartis: Other: personal fees; Bristol-Myers Squibb: Other: personal fees, Research Funding; Merck: Other: personal fees, Research Funding; Kite, a Gilead Company: Other: personal fees, Research Funding; Precision Biosciences: Other: personal fees, Research Funding; Legend Biotech: Other; Unum Therapeutics: Other, Research Funding; Acerta: Research Funding; Adicet Bio: Other; Allogene Therapeutics: Other: personal fees, Research Funding; Cell Medica/Kuur: Other: personal fees; Incyte: Other: personal fees; Poseida: Research Funding; Cellectis: Research Funding; Calibr: Other; Celgene: Other: personal fees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal